About 40% develop diverticulitis by middle age; men and women suffer the same. Nearly one third of all people with diverticular disorder will develop diverticular bleeding (a complication of diverticulosis and is more common in women), and 30% will eventually develop diverticulitis (a more serious form of diverticulitis).
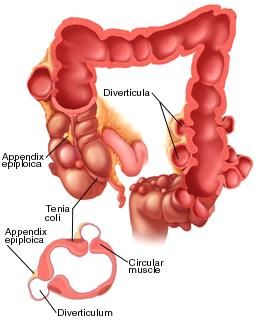
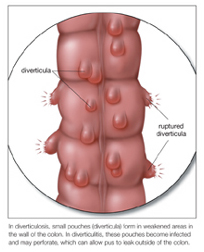
Diverticula are large, flat pockets (sometimes called pouches) of tissue, usually filled with fluid. Although abnormalities can be large or small, they are most commonly found in the lower colon. Diverticula are generally not harmful to the body; however, they can become serious health problems if left untreated. Diverticulopathy or diverticular bleeding is the most common cause of diverticula in the world.
When a diverticulum occurs, it means inflammation or infection of the tissues lining the colon. Bacteria (bacteria that naturally occur in the digestive tract and can also infect diverticula if present in large numbers) invade the intestinal wall. These bacteria then produce gases or wastes; these gases and waste products irritate the delicate lining of the intestines. This irritation causes irritation and inflammation, which in turn makes the white or yellow coating of diverticula, also known as mucus, more visible.
As soon as white blood cells are called to the scene to help the body fight the bacteria that cause inflammation, red blood cells in the bloodstream begin to attack the lining of the colon. In response to this rapid bombardment of blood, the immune system activates the production of white blood cells, which causes scarring and thickening of the colon lining. As the walls of the colon weaken, it becomes more difficult to absorb nutrients and eliminate waste. As a result, these diverticulopathy symptoms begin to appear. These symptoms may include: pain or burning, constipation, cramping or pressure, diarrhea, bloating, fatigue, itching, and gas (vomiting).
Deviation can be caused by many factors, from diet to unhealthy habits and even medications and diseases. Several treatments are available, but each person’s needs are unique. In some cases, surgery is the only effective treatment; in other cases, other methods may be used (for example, diet or medication changes).
One of the most common abduction treatments is the removal of diverticula. This is usually done surgically.
There are several surgical techniques, all depending on how much diverticular wall is left after surgery and the degree of damage. One of the simplest is laparoscopy, in which an endoscope is used to look at the colon, leaving a small opening in the anus. This allows the surgeon to examine the damaged area and make the necessary incision. Another method is the Roux enema, in which the surgeon injects a solution into the colon.
This type of surgery involves the use of a very strong fluid under pressure (propylene glycol or PEG, a mixture of water and ethylenediaminetetraacetic acid) that irritates the colon wall, causing it to collapse and remove material. Other types of surgical procedures used for abduction include sigmoidoscopy and pylori aspiration. However, surgery is not always the best option.
If diverticulitis is left untreated, symptoms are likely to return. For this reason, doctors recommend a combination of different methods, including dietary changes and medications. In addition, diverticulitis cannot be cured, but it can be significantly reduced and even eliminated. For example, if diet and exercise are combined with supplements that help prevent or stop the absorption of toxins, the likelihood of a second attack is reduced.
Some people choose to remove the diverticula by using a laser or surgical instrument. This is usually done only when the wall is very damaged and cannot be repaired, such as after surgery or cancer treatment. Although a laser may seem like a permanent cure, there is still hope for those with chronic diverticulosis. By changing their diet and getting plenty of rest and avoiding stress, they can greatly reduce the chances of a flare up.
Other people choose to try dietary changes, as well as herbal remedies and even dietary changes. Many recommend doing a liquid flush diet, a plan that combines a colon cleanse and a daily probiotic supplement. Others believe that taking special supplements containing natural fiber such as psyllium husk, or even chamomile tea can help reduce the severity of diverticulitis.
However, if diverticulosis symptoms persist or get worse after months or even years, it is time to see a doctor. Diverticulosis may be serious and require surgery. Although surgery is a permanent answer, there are other methods to treat the condition, including surgery and dietary changes. Surgery is not always the only answer.
